
For many women, the journey toward an endometriosis diagnosis begins long before they ever reach a gynecologist’s office. It often begins with severe menstrual pain in adolescence, persistent pelvic pain, or digestive issues, symptoms that have been dismissed, normalized, or misinterpreted for years.
Endometriosis is a condition in women, in which tissue similar to the inner lining of the uterus grows outside the uterus, often affecting the ovaries, fallopian tubes, bladder, bowel and tissue lining the pelvis. These growths, known as lesions or implants can also appear in unexpected places such as the lungs, diaphragm, or surgical scars. These lesions respond to hormones, especially estrogen. They thicken, break down, and bleed during the menstrual cycle, causing inflammation, scar tissue, adhesions, and severe pain.
Multiple studies have shown that endometriosis affects 1 out of 10 women. Yet, the average time from the onset of symptoms to a confirmed diagnosis remains 7 to 10 years, a delay that carries significant reproductive, psychological, and economic consequences. Understanding the reasons behind this delay is the first step toward taking action.
This article provides a detailed explanation for why endometriosis is hard to diagnose, what conditions commonly mimic endometriosis, and how to improve early detection.
There is no “single” known cause of endometriosis. However, research shows that the condition likely develops through multiple interacting factors including genetic, biological, hormonal, immune and environmental.
Endometriosis is not a single-gene disorder. It’s polygenic, meaning multiple genes contribute small influences that add up. And scientists have identified multiple genetic variants associated with immune regulation, hormone sensitivity and cell function. Research shows that endometriosis often runs in families, and having a close relative (mother, sister or aunt) with the condition significantly increases a person’s risk.
This occurs when menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body. This theory proposed by Dr. John Sampson in the 1920s suggests that this back flow of menstrual blood carries endometrial cells, which can implant in the pelvis and start growing, causing endometriosis.
But while Sampson’s theory is still widely cited, later research has shown that almost 90% of menstruating women experience some degree of retrograde flow, yet only a fraction develop endometriosis. This means retrograde menstruation alone cannot fully explain the condition.
Hormones, particularly estrogen, play a central role in endometriosis. High estrogen levels, or increased sensitivity to estrogen stimulates the growth of endometrial tissue, increasing pain and inflammation.
Additionally, progesterone resistance (a situation where the body is less responsive to progesterone), can promote uncontrolled tissue growth. While not a direct cause, hormonal imbalance plays a role in worsening the condition.
The immune system normally protects the body by identifying and removing abnormal cells, including endometrial cells that end up outside the uterus. But when there’s an immune system dysfunction, misplaced cells are allowed to survive and grow, resulting in endometriosis.
Endocrine disruptors such as Dioxins, Phthalates, BPA (Bisphenol A), can affect immune function, hormone regulation and cell growth. While they are not a primary cause, exposure to these chemicals or toxins can increase susceptibility in genetically or hormonally predisposed individuals.
In rare cases, especially after C-sections, or Hysterectomies, endometriosis can occur in surgical scars. This happens when endometrial tissue is accidentally transferred to the surgical incision site, where it implants and grows.

Source: Pinterest
Several factors contribute to prolonged endometriosis diagnosis including:
Although endometriosis is common, many primary care providers (PCPs) receive limited training on identifying early symptoms, recognizing non-classic presentations and effectively treating the disease. This has resulted in misdiagnosis and subsequent incomplete treatment.
Without grounded gynecology training, endometriosis is not always considered as a first or even second possibility. Why? The main symptom of endometriosis is pelvic pain often associated with menstrual periods. Although many people experience menstrual cramps, for people with endometriosis, the pain is far worse than normal.
Unfortunately, menstrual pain is commonly dismissed as routine, particularly in young women. This normalization results in delay in seeking medical attention and missed opportunities for early diagnosis. And PCPs may unintentionally contribute to this when they reassure patients that “painful periods are common” without conducting further assessment.

Source: Pinterest
Endometriosis does not manifest uniformly. Symptoms differ based on lesion location, depth, and individual pain sensitivity. Some patients experience mild pain despite extensive disease, while others have significant symptoms with minimal visible lesions.
Common symptoms of endometriosis include chronic pelvic pain, excessive bleeding and severe menstrual pain (Dysmenorrhea), painful intercourse involving vaginal penetration, painful bowel movements, painful or frequent urination, gastrointestinal issues, fatigue, back pain. Disease progression can lead to organ dysfunction and infertility.
However, the major reason endometriosis is underdiagnosed is that it mimics multiple other disorders such as Pelvic inflammatory disease, Irritable bowel syndrome (IBS), Urinary Tract Infections (UTIs), Ovarian cysts, Fibroids, Painful bladder syndrome or Appendicitis.
The fact that endometriosis symptoms widely overlap with symptoms of these conditions complicates early recognition and significantly prolongs the differential diagnosis of endometriosis.
For decades, medical studies used male subjects as the default. This practice has followed a consistent pattern. Women’s pain is often underestimated, misinterpreted, or dismissed compared to men’s pain, resulting in the understudy of female-specific pain disorders.

Source: Unsplash
Many women with endometriosis start reporting severe menstrual pain in their adolescence. But instead of being investigated, their pain is often described as “normal period pain” or “low pain tolerance”.
Pelvic pain has been themed as “part of womanhood”, so even when the pain is debilitating, affecting school or work, it is still underestimated by many health practitioners.
This normalization of women’s pain delays referral to a gynecologist and further prolongs diagnosis.
The lack of an accurate endo endometriosis symptoms test contributes heavily to underdiagnosis. Despite ongoing research, no blood test, biomarker, or imaging modality reliably detects early or superficial lesions. Overtime, pelvic examination, CT, ultrasound and MRI have been used for screening, but studies prove that none of these tools can accurately confirm and diagnose endometriosis.
For example, ultrasounds only detect ovarian endometriosis, not the majority of endo lesions, while pelvic exams and MRI only detect advanced-stage disease. The most definitive endometriosis diagnosis tool is laparoscopy, often combined with biopsy.
Diagnostic laparoscopy is a minimally invasive surgery that allows a surgeon to look inside the abdomen and identify lesions or scar tissue.
While laparoscopy allows for direct visualization and potential excision, doctors are often reluctant to recommend it early due to the involvement of surgery, limited access to skilled excision surgeons and cost-related barriers.
Endometriosis diagnosis requires specialist care, repeated appointments, and in many cases diagnostic laparoscopy, procedures that are difficult for patients with limited financial resources.
In the U.S., the healthcare system is largely insurance-based, costly, and fragmented. Inadvertently, women with lower income, unstable employment, or limited access to healthcare, experience significant delays in getting medical evaluation or diagnosis and treatment.
Endometriosis is not widely discussed in schools, workplaces, or even within families. Many people don’t know the early warning signs. Others have never heard the term “endometriosis” until adulthood. People assume their pain is caused by stress, infections, or lifestyle changes instead of a chronic condition. And since menstrual and pelvic pain are rarely openly discussed, some women feel embarrassed bringing up their symptoms.
Many people are unable to differentiate between “normal” and “abnormal” menstrual pain. A lot of women and girls grow up being told that painful periods are “just part of being a woman.” As a result dysmenorrhea is normalized, intense pelvic pain is dismissed as something that should be tolerated and symptoms go unreported for years.
Without understanding the condition, individuals can’t advocate for themselves or ask the right questions at appointments.
Endometriosis cannot be prevented, but research shows that certain modifiable lifestyle and medical factors may reduce the risk, delay progression, or lessen severity. These are not cures, but they may help lower the likelihood of developing endometriosis or prevent it from worsening.
Manage estrogen levels by engaging in regular physical activity to maintain a healthy weight, and reducing alcohol intake.
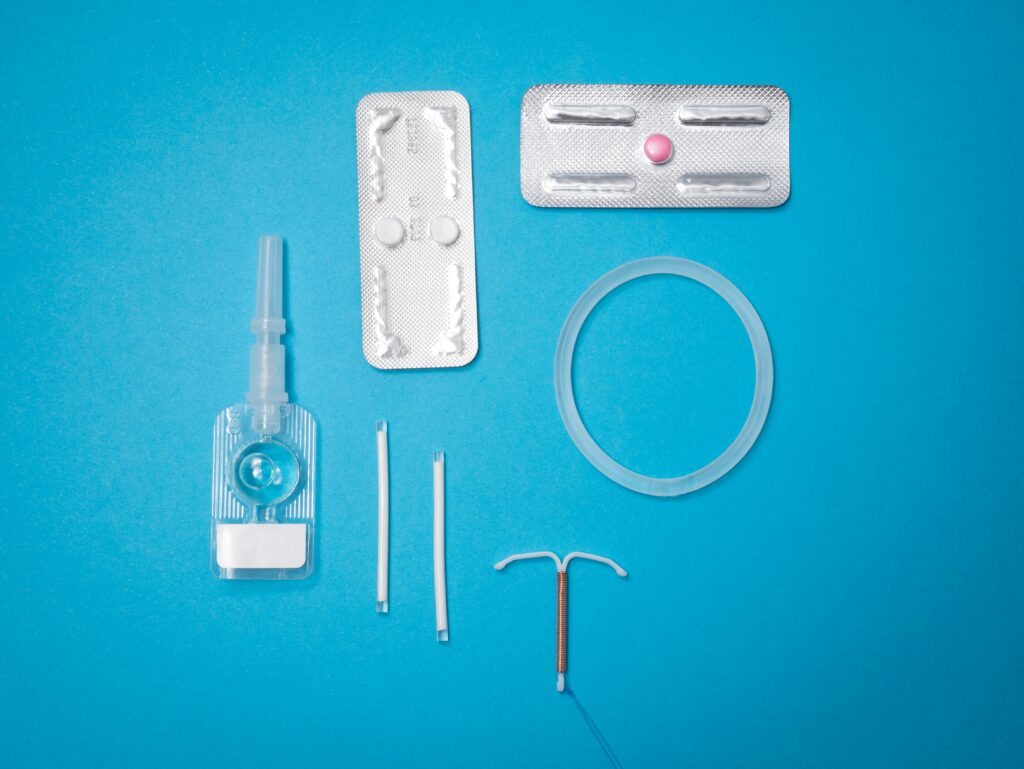
Hormonal treatments using oral contraceptives or insertion of hormonal intrauterine device (IUD) can help suppress ovulation and menstruation, lowering the risk of formation or progress in growth of endometrial implants.
Source: Unsplash
Certain dietary patterns may reduce chronic inflammation, which may support overall pelvic health. Helpful choices include eating more fruits, vegetables, whole grains, and omega-3–rich foods (like salmon and walnuts), reducing consumption of red meat and processed foods.
Reducing exposure to endocrine disruptors found in plastics, pesticides, and chemicals, may help lower risk, especially in genetically predisposed individuals.
Avoiding unnecessary abdominal or pelvic procedures may lower the risk of surgical transplantation of endometrial tissues.
Knowing your family medical history helps in early detection and treatment of menstrual irregularities, preventing long-term complications like infertility or chronic pelvic pain,
The prolonged wait for an endometriosis diagnosis is a structural and clinical challenge that can be improved with awareness, training, and research. And though no treatment permanently cures endometriosis, recognizing the condition’s complexity, prioritizing early evaluation, and validating patients’ pain are essential to reduce the diagnostic gap and prevent disease progression.